CRPS is an unusual pain disorder that often develops after surgery or injury. It can be acute (under 6 months duration) or chronic (over 6 months).
Signs and Symptoms
CRPS is characterised primarily by a constant pain, which seems to be more extreme than it should given the recent history.
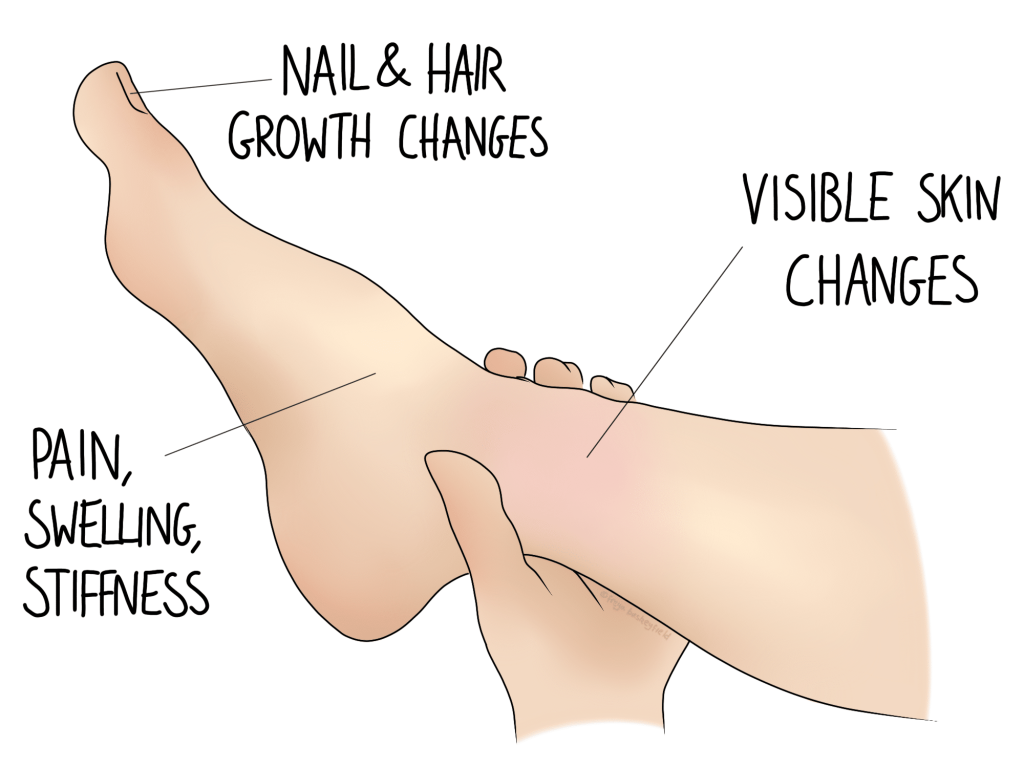
Unlike other pain conditions, CRPS causes signs that are apparent to other people, not just the person suffering with it. The affected limb may:
- be hot or cold to touch
- sweat more than the rest of the body
- swell
- grow or lose hair
CRPS, although featuring some objective signs, is a functional illness. This means that it’s not a collection of signs and symptoms that leads to the diagnosis, rather it’s the absence of them that excludes another diagnosis. This is known as a diagnosis of exclusion, which is the same process used to rule out other conditions to conclude that someone has IBS.
However, the Budapest Criteria has been developed to help to point a diagnosis towards CRPS where appropriate. The criteria considers:
- the presence of the signs mentioned above
- the presence of constant, high level pain
- whether another condition could explain the symptoms (other tests may still need to be performed)
Why Does CRPS Happen?
Unfortunately, this condition is very poorly understood. It does share features with other pain conditions, which is helpful for the development of management strategies.
Pain does not exist in a vacuum. It is an experience built on factors such as
- biological injury
- expectation and understanding
- fear for how it will affect you
This is not to say that your suffering is self inflicted, rather that better understanding can be one very powerful way to start improving your symptoms. We can help with this.
9/10 cases of CRPS follow surgery, and of those following injury, most are attributed to workplace injury. Although this correlation may seem suspicious, it is more likely associated with the fear that pain will limit work and income, or other stressors.
Osteopathy and CRPS
If you come to your appointment without a diagnosis, our first job will be to ensure that the problem is not out of our remit. This may warrant further investigation such as x-rays or blood tests before we know that you’re safe to treat. CRPS can present like a frozen shoulder, arthritis, or bad sprain initially, so we will continue to monitor your progress as you move through the management plan. If you have already been through the system, we can get started straight away, in association with your other medical professionals.
The current UK guidance is that management strategies should comprise of 4 pillars:
- Physical and vocational rehabilitation
- Psychological intervention
- Information and education to support self management
- Pain relief in the form of medication and procedures
Your osteopath is equipped to support you through pillar one: physical rehabilitation, and pillar 3: information. These pillars may include graded exposure therapies to reduce sensitivity. They may also involve strengthening and other exercises, and techniques to improve mobility. Treatment is often wide reaching to help to take the strain off the affected area by improving function elsewhere.

