

Sometimes patients will mention that they have a family history of arthritis, but they’re not sure if it’s rheumatoid arthritis (RA) or osteoarthritis. Full diagnosis of RA usually requires a blood test or imaging from your GP or rheumatologist. But there are a few points that set RA and OA apart that we can identify in clinic.
RA often starts earlier in life than OA, but there is some overlap. Symptoms can start anywhere between the late 20s and 50s. OA could start in this window too, but often there is an underlying injury that causes increased demand on the joint that becomes arthritic.
Small joints are typically affected first by rheumatoid arthritis: joints of the hands, feet, and neck might show the first signs. Localised achiness is common, but as the condition is autoimmune, there might also be more generalised symptoms. Feeling generally under the weather or fatigued can be the result of a rheumatoid arthritis flare. Due to the inflammatory nature of the condition, pain is often worse after rest or intensive exercise. Morning stiffness that lasts more than 30 minutes should be investigated by your osteopath or GP. Ice is often quite soothing for inflammatory pain, but avoid direct contact with the skin, or application for more than 10 minutes per hour.
Osteoarthritic pains frequently affect larger joints, such as the hip and knee. These too may be worse after too much movement or first thing in the morning. However these symptoms often clear quickly with movement, and should not cause more than half an hour of discomfort in the early stages. We can also help you to manage osteoarthritis.
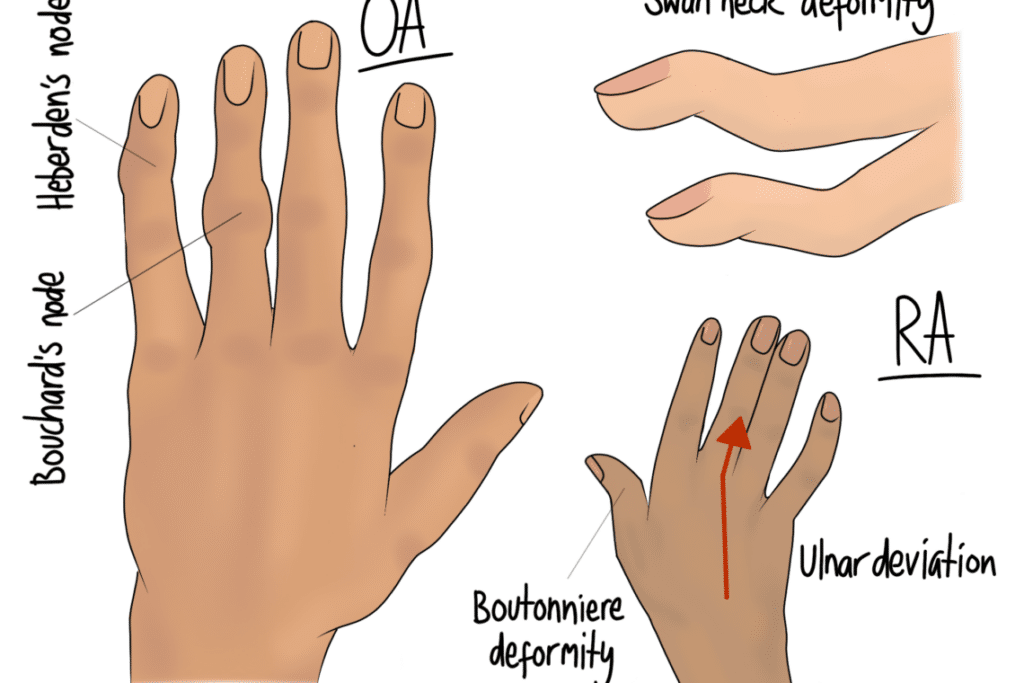
After many flare ups, the affected joints can be structurally altered. The hands often show this clearest. Again, both RA and OA can cause hard swellings on the knuckles and finger joints, but RA can also cause a “swan neck” deformity or ulnar deviation (both illustrated above). These signs point quite clearly to rheumatoid arthritis.
Osteopaths are qualified to help manage arthritic and rheumatic pains. However, we cannot prevent the flares that cause damage over time. This is why it is important for us to work alongside your GP and rheumatologist. Medication is often the most effective part of your treatment plan, working to prevent or minimise the flares and the damage they can inflict. Diagnosis might follow a blood test to identify inflammatory or autoimmune markers. Sometimes imaging is also appropriate for certainty. Note that not all “full” blood tests that you might have had for other reasons would show the markers that are tested in an RA blood test.
The changes to affected joints can cause instability and hypermobility. This can be a cause of neck pain between flare ups, as the muscles of the neck have to work harder to keep the area stable. We can help manage this discomfort, providing exercises to strengthen the muscles so that they can manage the increased demand. Your osteopath will also look elsewhere in the body to check that other areas are working well, and not putting yet more demand on the neck.