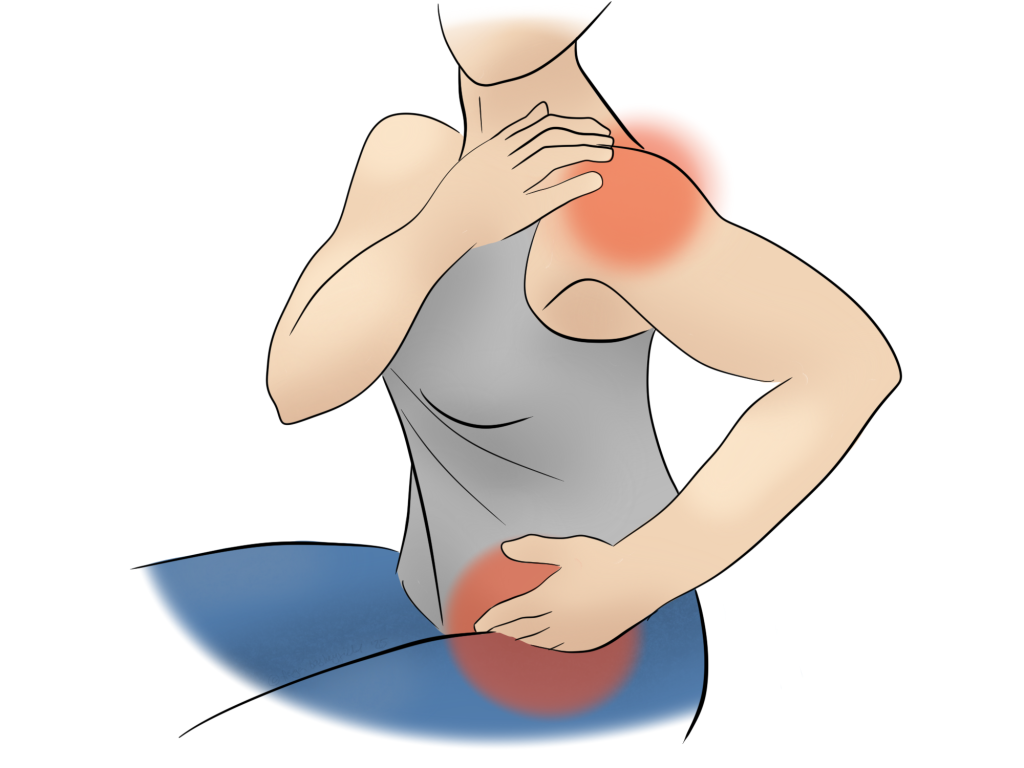
PMR is an autoimmune condition that causes pain the shoulders and hips. It has a lot of similarities to other conditions like rheumatoid arthritis, but it needs diagnosing accurately to get your the most effective treatment.
What is PMR?
Polymyalgia Rheumatica is a descriptive name. It means “multiple joint pain of rheumatological origin”. The multiple joints in question are typically the hips and shoulders. Neck pain can occur too, but this might be more indicative of Temporal Arteritis (not arthritis). This is a condition where arteries become inflamed in roughly 20% of PMR patients. It causes headaches and neck pain, but can cause more serious issues associated with blood supply to the brain, so should be investigated quickly.
As with a lot of rheumatological conditions, PMR affects more women than men, and peaks around the age of 60. It’s not clear what causes it, but it’s likely a mixture of genetic and environmental factors. Sometimes rheumatological conditions follow some sort of trauma, but this is not always the case. However, it can make the signs easier to miss if it looks like an injury with a clear onset.
Management
Standard treatment during a PMR flare up is a course of steroids. For some people, this has a quick effect in getting their pain and mobility back to a normal level. But other people might continue to struggle for a while. In these cases, your GP may like to increase the dosage for a while before tapering off. It’s not uncommon to remain on prednisolone for a year or two to keep symptoms controlled.
Osteopaths are well placed to help manage the painful symptoms of a number of rheumatic conditions. Even when the inflammation is under control, muscles can remain tight and cause pain and stiffness locally and further afield. We can work to restore your mobility by encouraging muscles to relax and joints to move smoothly again.
Osteopathy and PMR
Effective management of PMR requires a visit to your GP to access those steroids. But your osteopath is well placed to flag your symptoms as rheumatological. If you present with:
- an inflammatory pattern, such as morning stiffness that lasts over 30 minutes
- symmetrical symptoms
- new headaches, that might be associated with jaw pain
Your osteopath will think about referring you back to your GP. Signs of temporal arteritis warrant a more urgent visit to the GP, or a call to 111 if you can’t get in with them.
As mentioned above, we can use our usual techniques to encourage joints to move better after a flare. If you develop compensatory patterns that lead to other aches and pains too, we can help with those as well. Sometimes tension around the hips extends to the buttock muscles, and can catch the sciatic nerve. That’s one more ache you don’t need, and don’t have to suffer with! Treatment to restore balance after periods of tension can help to get you back on track quicker.
Click here to make an appointment for your pain in Leicestershire or Rutland